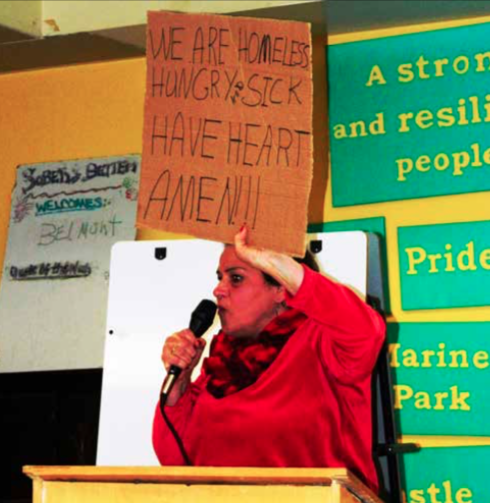
Late December 2017, Kindred Healthcare announced it was closing, among other Care Facilities in its network, the Harbor Lights Rehabilitation Home located on Columbia Road South Boston. Lawmakers, including Senator Nick Collins, called for an investigation by the Attorney General of MA, Maura Healy, over the unexpected closing, on the heels of the organization’s 2016 lobbying for state funds to underwrite employee compensation. The status of that investigation is unclear, but, this week, the Boston Globe reported that rest homes are closing, home care oversight questioned, nursing homes need more money and private pay facilities are too expensive for those who need affordable care.
The pressure, as usual, is on those least able to afford the costs of health care. 73 rest homes operate across the state . They trace their roots to the 19th century, when fraternal, religious, and ethnic groups pooled their funds to furnish large Victorian homes to provide for needy widows in an era before Social Security. Those that endure remain a vital safety net for low-income older residents, many of whom have mental or behavioral disabilities. Two dozen rest homes have closed in the past decade alone. One in Western Massachusetts was converted to a doggie day care.
But as new assisted-living complexes have opened, drawing more affluent residents, they’ve left the rest homes with a majority of residents on public assistance. At the same time, more resources have been funneled to helping older residents stay in their homes. As a result, the number of beds at Massachusetts rest homes has fallen 57 percent, from 7,000 to 3,000, since 1998. Operators lament that it’s very difficult to run a business in 2018 based on 2012 costs. The Baker administration is trying to remedy the reimbursement formula to provide some amount of support.
Home health care has been the go-to option for many, especially the middle-income families. But a Globe series reported on the lack of oversight to keep seniors safe and properly cared for. Among the red flags raised by the series are that a lot of personal care aides, specifically those in Massachusetts, are not undergoing background checks or receiving training before they are tasked with a caregiving job. Home health aides and personal care aides are estimated to account for 41% of job growth by 2026, according to the Bureau of Labor Statistics.
In Massachusetts, anyone can become a home care worker and work privately, though state law does require home care agencies to perform background checks. Personal care attendants hired through a MassHealth program are required to attend a state-run three-hour orientation session. In addition to outlining oversight issues, The Boston Globe also reported on the influx of immigrants in the home care industry, specifically highlighting a growing number of workers in Massachusetts who emigrated from Ghana.
The Home Care Alliance of Massachusetts has vigorously pushed back and released a statement in response to The Boston Globe series stating that the articles failed to properly explain the home care system in the state and left readers scared and confused. Their guidelines state that The Home Care Alliance and its members have a zero-tolerance policy when it comes to patient abuse.
Over many years The Alliance has worked with the Department of Public Health, Elder Affairs and Health and Human services to address issues of elder abuse and billing fraud. Their members take very seriously the responsibility of ensuring the safety and quality of care being delivered to their clients. While the Globe article cites 20 cases of agency-hired workers committing abhorrent crimes in recent years, it fails to contextualize the fact that home care agencies have employed over 75,000 workers and delivered care to more than 600,000 elders in the past five years.
Home care agencies are not the only home-based providers drawing scrutiny for lack of oversight. Federal watchdogs have repeatedly stated their intentions to continue investigating the hospice industry for fraud, waste and abuse. Health care is front and center, and the system is teetering on the brink of a ‘financial breakdown’, if the layers of care are not reimbursed commensurate with the obligation of government reimbursement and the reality that costs must address each layer fairly, and not just underwrite those who can afford expensive and influential lobbyists.